A Solitary Confinement
A true story about Guillain-Barre Syndrome by
Robin Sheppard
A true story about Guillain-Barre Syndrome by
Robin Sheppard
June, 2024
Guillain-Barré syndrome (GBS) is a rare condition in which the immune system mistakenly attacks the nervous system, leading to muscle weakness, numbness, and paralysis.
Guillain-Barré syndrome (GBS) starts suddenly and can get worse over hours, days, or weeks until specific muscles can’t be used at all. Some GBS cases are very mild and only cause brief weakness. Others lead to almost complete paralysis, making it impossible for the person to breathe on their own. In these cases, the condition is life-threatening and could affect breathing, blood pressure, or heart rate. However, most people eventually recover from even the most severe cases of GBS. After recovery, people may still have some weakness.
Symptoms of Guillain-Barré syndrome
Who is more likely to get Guillain-Barré syndrome?
Guillain-Barré syndrome is an illness that can affect anyone, but it most commonly impacts adults and individuals over the age of 50. It is not contagious or inherited, and the exact cause is unknown.
Guillain-Barré syndrome is an autoimmune disease where the immune system mistakenly attacks healthy nerves, possibly triggered by a response to an infection. This occurs because certain chemicals in bacteria and viruses resemble those in nerve cells, causing the immune system to target healthy nerve cells.
The body’s nerves have a central core called the axon surrounded by an insulating layer called myelin. In most cases of GBS, the immune system damages the myelin sheath, affecting the transmission of nerve signals and causing muscle weakness.
Guillain-Barré syndrome often starts after a respiratory, gastrointestinal, bacterial, or viral infection. It can be caused by Campylobacter jejuni bacteria, surgery, or, in rare cases, certain vaccines. In some cases, COVID-19, Zika, cytomegalovirus, or Epstein-Barr viruses have also been linked to GBS.
Diagnosing Guillain-Barré syndrome
Currently, GBS has no cure. However, certain treatments can lessen its severity, shorten recovery time, and address the disease’s complications.
People with Guillain-Barré syndrome are usually admitted to the hospital and treated in the intensive care unit due to possible complications of muscle weakness. At the hospital, they will be closely watched to track the progression of their muscle weakness, breathing, and heart rate. If they need help, the hospital staff can quickly provide it.
When dealing with paralysis, it’s essential to provide supportive care to address complications as the body recovers. Keep a vigilant watch on breathing, as respiratory failure is a potential risk in cases of GBS. A mechanical ventilator may sometimes be necessary to support or control breathing. Monitor the autonomic nervous system, which regulates the functions of internal organs and some muscles in the body. Changes in heart rate, blood pressure, digestion, or sweating may occur, so the person should be put on a heart monitor or other equipment that measures and tracks body function. If the person has problems swallowing, they may also need special care to prevent choking, which can cause pneumonia.
Once individuals with GBS show signs of improvement, they may be moved from the acute care unit in a hospital to a rehabilitation facility. Here, they can work on rebuilding their strength, undergo physical rehabilitation, and receive other therapy to help them return to their daily activities.
GBS can affect different body parts, so preventing or treating complications may require various methods. For example, a physical therapist can move and position the person’s limbs to maintain muscle flexibility and prevent muscle shortening. Stronger muscles may take over the function of weaker ones—a process known as substitution. A physical therapist can choose specific exercises to strengthen weaker muscles so they can regain their original function.
Occupational and vocational therapy helps people learn new ways to handle everyday tasks and work demands, as well as the need for assistive devices and other adaptive equipment and technology.
GBS can be a severe illness because it causes sudden and quick onset of weakness—and often paralysis. Fortunately, most people with GBS fully recover.
Recovery from GBS can take a long time, ranging from a few weeks to a few years. Some people may not fully recover and experience long-term weakness, numbness, fatigue, or pain. Adjusting to sudden paralysis and needing help with daily activities can be very challenging. Some people may also need mental health counselling to help them cope. Support groups can provide emotional support and valuable information to those recovering from GBS.
Conclusion
People diagnosed with Guillain-Barré Syndrome (GBS) often don’t know how the condition will progress. GBS is unpredictable and can cause a wide range of symptoms, making it hard to predict what will happen to each person. Some people with GBS get much better over time, while others may have long-term problems.
People with GBS should work closely with their healthcare team to manage ongoing symptoms and improve their overall well-being. Supportive therapies like physical, occupational, and psychological support can help. It’s important to actively participate in your care, talk openly with healthcare providers, and change treatment plans as needed.
By doing so, individuals with GBS can navigate the uncertainties of the condition and work towards achieving the best possible outcome for their health and quality of life.
Furthermore, for those seeking inspiration and insight into overcoming GBS, consider exploring “A Solitary Confinement: Always look on the bright side, even though you’re paralysed from the neck downwards” by Robin Sheppard, who recovered from this disease.
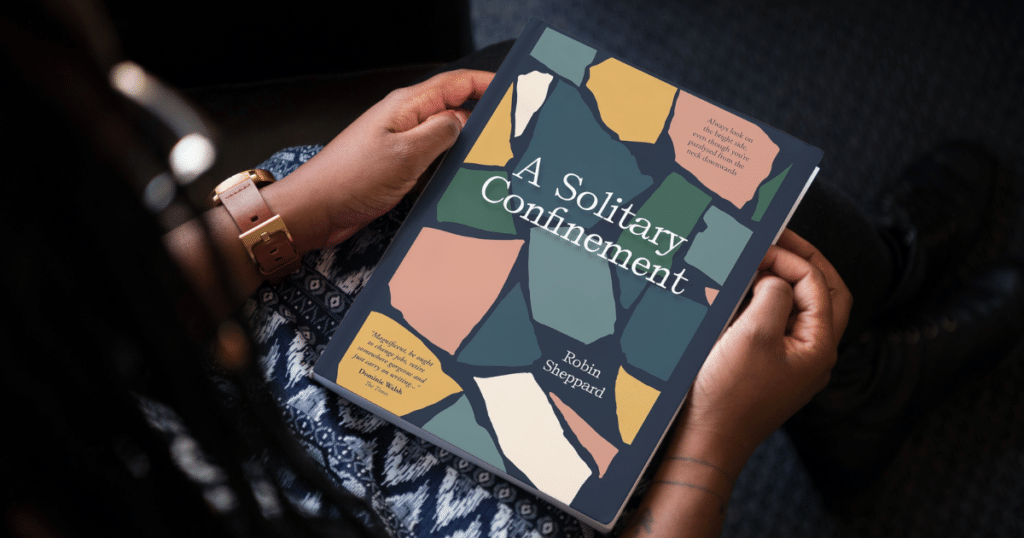
This book offers a firsthand account of triumph over adversity, providing valuable perspectives and encouragement for individuals facing similar challenges. By embracing a proactive approach to managing GBS and seeking support from healthcare professionals and inspirational resources like this book, individuals can strive towards achieving the best possible outcome for their health and quality of life.
Don’t wait; start your journey of resilience today! Click HERE!